Volume 20, Number 5—May 2014
Research
Abstract
We conducted a study to determine prevalence of
HPV types in oropharyngeal cancers in the United States and establish a
prevaccine baseline for monitoring the impact of vaccination. HPV DNA
was extracted from tumor tissue samples from patients in whom cancer was
diagnosed during 1995–2005.
The samples were obtained from cancer
registries and Residual Tissue Repository Program sites in the United
States. HPV was detected and typed by using PCR reverse line blot
assays.
Among 557 invasive oropharyngeal squamous cell carcinomas, 72%
were positive for HPV and 62% for vaccine types HPV16 or 18.
Prevalence
of HPV-16/18 was lower in women (53%) than in men (66%), and lower in
non-Hispanic Black patients (31%) than in other racial/ethnic groups
(68%–80%).
Results indicate that vaccines could prevent most
oropharyngeal cancers in the United States, but their effect may vary by
demographic variables.
Oropharyngeal cancers include malignancies that occur
where the oral cavity and pharynx merge, including in the palatine and
lingual tonsils, the posterior 1/3 (base) of the tongue, the soft
palate, and the posterior pharyngeal wall.
Current worldwide incidence
has been estimated at ≈85,000 annually (1),
although it varies extensively by geographic region.
In the United
States, ≈12,000 new oropharyngeal cancers are diagnosed annually (2);
most are classified histologically as squamous cell carcinoma (OPSCC).
In addition to tobacco use and alcohol use, infection with human
papillomavirus (HPV) has been recognized as an independent risk factor
for oropharyngeal cancer (3–6).
The 2 HPV vaccines approved by the US Food and Drug Administration
protect against infection with HPV-16 and HPV-18, which are the
high-risk types most frequently associated with cervical cancer.
A
candidate 9-valent vaccine that includes types in the existing
quadrivalent vaccine (HPV types 6, 11, 16, and 18) and 5 additional
high-risk types (31, 33, 45, 52, and 58) is in clinical trial.
Supported
by evidence that existing vaccines effectively reduce oral HPV
infections, these formulations may also reduce incidence of
oropharyngeal cancers (7).
When monitoring the population-level effect of HPV vaccination on
oropharyngeal cancer occurrence in the United States, data on the
incidence and type-specific prevalence of this disease are essential.
Previously, the prevalence of cases attributable to viral infection and
the consequent effects of vaccine programs were approximated from small
published studies (8–13),
which estimated HPV to be detected in 37%–60% of OPSCC in North
America.
Considering the range of prevalence, the heterogeneity of study
populations, and differences in sample preparation and HPV detection
methods used in these studies, it is not clear that this range of
estimates reflects the true scope of HPV-associated OPSCC in the United
States.
Therefore, the objectives of this study were to determine
prevalence of HPV types detected in oropharyngeal cancers in the United
States and to establish a prevaccine baseline for monitoring the impact
of vaccination.
Materials and Methods
Cancer Tissue Specimens
As part of the Centers for Disease Control Cancer Registry Sentinel Surveillance System study (M. Saraiya, unpub data), a systematic review of cases of oropharyngeal cancer diagnosed during 1995–2005 was performed.The cases were selected from 7 participating registries, including 4 central cancer registries in Florida, Kentucky, Louisiana, and Michigan and 3 Surveillance, Epidemiology, and End Results program (SEER [http://seer.cancer.gov/
The following anatomic regions (by ICD-O-3 codes) were included: C01.9 and C02.4 (base of the tongue and lingual tonsil); C09.0, C09.1, C09.8, C09.9, and c14.2 (tonsil); C14.0, C14.2, C14.8, C02.8, C10.2, C10.8, and C10.9 (other oropharynx) (13). Of 4,073 cases matching these criteria, we requested samples from 1,271 case-patients representative of the whole case-patient population regarding sex, age, and race/ethnicity.
One archived, formalin–fixed paraffin-embedded tissue sample, representative of the primary tumor, was selected by the submitting pathology laboratory.
If tissue from the primary tumor was unavailable, a sample from a metastatic lesion in a lymph node was accepted because HPV prevalence is usually maintained in OPSCC–positive lymph nodes (14).
With the exception of 32 cases from Hawaii and 11 from Los Angeles County, which had been sampled by Chaturvedi et al. (12), cases were selected exclusively for this study.
Each participating state and CDC received approval from their institutional review boards for the study; CDC approved the overall study.
DNA Extraction and HPV Typing
All laboratory methods were described previously (15,16).Six consecutive 5-μm sections were cut from each selected tissue block; special precautions were used to avoid cross-contamination.
The first and last sections were stained with hematoxylin and eosin and reviewed by a study pathologist (ERU) to confirm the presence of viable tumor tissue.
DNA was extracted from two 5-μm sections by using high temperature–assisted tissue lysis (17) and further purification was carried out by automated extraction by using Chemagic MSM1 (PerkinElmer, Waltham, MA, USA). HPV types were determined from 2 commercial assays by using an algorithm which was evaluated earlier for this application (18,19).
First, all DNA extracts were tested by using the Linear Array HPV Genotyping Assay (Linear Array; Roche Diagnostics, Indianapolis, IN, USA) and a HPV-52-specific PCR to resolve ambiguous positive results from the XR probe of the Linear Array HPV test (20).
Samples that had negative or inadequate linear array results (negative for HPV and cellular β-globin controls) were retested with the INNO-LiPA HPV Genotyping Assay (Innogenetics, Gent, Belgium).
HPV status was recorded for 40 types: 6, 11, 16, 18, 26, 31, 33, 35, 39, 40, 42, 43, 44, 45, 51, 52, 53, 54, 55, 56, 58, 59, 61, 62, 64, 66, 67, 68, 69, 70, 71, 72, 73, 74, 81, 82, 83, 84, IS39, and 89 as tested; and HPV of an unknown type (HPV-X) for additional unspecified types as indicated by LiPA results.
Analysis
Prevalence was assessed as percentage positive from the total number of cases with valid results.HPV types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68 were considered to have a high risk for oncogenic potential (21) and all other types, including HPV-X, to have a low risk, showing low or no known oncogenic potential.
Hierarchical categories for HPV status were assigned as follows: HPV-16 includes all cases positive for this type regardless of other results.
HPV-18 includes all cases positive for HPV-18, but not for HPV-16; other 9-valent, high-risk HPV types included in the next generation of the HPV vaccine:
HPV-31, -33, -45, -52, -58, but not HPV-16 or -18; other high-risk HPV cases positive for any high risk not included in the previous categories:
HPV-35, -39, -51, -66, -68; and
low-risk HPV: all other cases positive for any remaining low-risk HPV types.
Statistical analysis was restricted to case-patients that had confirmed invasive OPSCC. Case-patient age at diagnosis was stratified into 4 groups: <50, 50– 59, 60–69, and >70 years.
Cancer stages were crudely classified as local, regional, or distant (metastatic) by SEER classifications.
Differences in prevalence of positive results for high-risk HPV or HPV-16/18, categorized by patient’s age, sex, race/ethnicity, and the anatomic location of cancer, were evaluated by using the χ2 or Fisher exact test whenever possible.
Multivariate analysis was performed by using logistic regression with a step-down procedure, adjusting for age, sex, and race/ethnicity as appropriate.
All statistical calculations were made by using SAS 9.3 (SAS Institute Inc., Cary, NC, USA).
Results
Those not received were either unavailable or the remaining tissue was not representative of disease.
The demographic characteristics (sex, age) and cancer stage (Table 1) (22) of the cohort from which the tested sample set was collected were similar to those of the untested cohort.
Persons from the Asian Pacific Islands were few in number and slightly overrepresented in the final test population.
HPV results for 476 (81.0%) samples were from the linear array and 112 (19%) from LiPA.
Most tissue was from the primary site (n = 473), but for 15 samples, only metastatic tissue from lymph nodes was available.
Most case-patients (77.6%) were from urban areas or counties with a population >250,000.
Most (94.4%) diagnoses were made during 2000 or later.
Median age at the time of diagnosis was 58 (range 28–97) years.
The male-to-female ratio was 3:1 and most of the cases (75.6%) were in non-Hispanic White persons.
SCC, the most common histologic type of oropharyngeal cancer, accounted for 557 (94.7%) of all cases, and the main analysis was restricted to these cases (Table 2).
HPV was detected in 403 of the 557 OPSCC cases (72.4%) with valid typing results and 396 (71.1%) were positive for >1 high-risk type (Table 3).
In 68.4% of cases, a single HPV type was found; 3.9% contained 2 types.
In 7 cases, only low-risk HPV types were detected: HPV-11, 26, 69, 82 (2 cases), 83, and HPV-X). HPV-16 was present in 337 (60.5%) cases, HPV-18 in 14 (2.5%) cases, and 331 (59.4%) cases were exclusively positive for these 2 types.
Other high-risk types, including HPV-31, 33, 35, 39, 45, and 52, were found at low frequency (Table 3).
The relative prevalence in case-patients that had multiple HPV types essentially followed single–type distributions.
HPV-16/33 was the most frequent combination (6 cases); HPV-16/18 and HPV-16/31 were the next most frequent, found in samples from 3 case-patients each. Frequencies of all co-detected HPV types are shown in Table 4.
More than 2 types were not found in any of the oropharyngeal cancers.
Proportions of high-risk HPV prevalence and HPV-16/18 were statistically different among the registries and by race/ethnicity, stage, and anatomic subsite (Table 2).
By sex, prevalence was only different for those infected with HPV-16/18.
Age at diagnosis was not statistically different between the stratified groups, but median age at diagnosis among high-risk HPV positive case-patients was 58 (28–92) years and 61 (36–97) years in high-risk negative case-patients (p = 0.023).
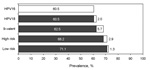
According to hierarchical assessment, HPV-16 was found in 337 (60.5%) OPSCC cases, HPV-18 in 11 (2.0%), other 9-valent high-risk types in 32 (5.7%), other high-risk types in 16 (2.9%), and low-risk types in the remaining 7 (1.3%) cases (Figure 1).
Of the 15 case-patients for whom lymph node metastases were tested, 14 were positive for high-risk HPV and 13 were positive for HPV-16.
In multivariate analysis for high-risk HPV that included age and sex in the model, only race/ethnicity was a significant independent factor (p = 0.003).
Odds for high-risk HPV infections were significantly higher for all other race groups than for non-Hispanic Black persons (p<0.001).
When only HPV-16/18 detection was considered, significant differences were found in sex (p = 0.009) and race/ethnicity in (p<0.001), but not age (p = 0.063), between those infected and those who were not (Table 5).
The 31 cases that had histologic results other than SSC included 7 adenocarcinomas (2 were HPV-16 positive, 5 HPV negative) and 2 small cell or neuroendocrine carcinomas (both HPV negative).
Twenty-two cases were carcinomas not further specified, of which 7 tested positive for HPV (4 for HPV-16, and 1 each for HPV-18, HPV-33, HPV-35).
Discussion
In a systematic review of HPV prevalence studies, including several small investigations of populations in North America, Kreimer et al. estimated that 47% of OPSCC cases were HPV related (11).
Chaturvedi et al. more recently estimated weighted HPV prevalence at 72% (12), which is comparable to our findings.
A continuous increase in HPV-related OPSCC that was observed during the past 20 years and escalated after 2000 (23) may explain some of the discrepancies found in the literature.
More sensitive laboratory methods may also have contributed to the increased HPV prevalence relative to earlier investigations.
All studies in North America considered by Kreimer et al. (11) relied on the MY09/11 or GP5+/6+ consensus primer sets that require intact HPV L1 fragments of 450 and 150 bp, respectively.
By contrast, in the study by Chaturvedi et al. (12) and ours, testing incorporated the INNO-LiPA assay, which has SFP primers that target 65-bp amplicons.
Assays targeting smaller L1 amplicons can achieve increased sensitivity for HPV detection in formalin-fixed, paraffin-embedded tissues known to have smaller DNA templates in their extracts than fresh or frozen samples do (18).
Although not identical in specificity to that of the Linear Array, INNO-LiPA had shown comparable performance for detecting single type HPV infections predominantly found in cancer tissues (19).
Our current study results further confirm a trend of increasing incidence of tonsillar cancers with shifting demographic patterns (24,25).
The results further confirmed that HPV-16, detected in 84% of all positive tissues, was by far the most frequent type found in oropharyngeal cancers.
Although type 16 also has nominally the highest prevalence in the “normal” oral cavity or oropharynx, other types are usually found at similar frequency (26,27).
The ability of HPV-16 to establish persistent infection and its potential to transform might be responsible for its prominence in cancers.
Currently available HPV vaccines targeting HPV-16 and -18 may be highly effective against OPSCC (9).
A candidate 9-valent vaccine (currently in clinical trials) could have the potential to prevent virtually all HPV-associated oropharyngeal cancers: our data showed that 2.9% of the case-patients were positive for a high-risk type not covered in this formulation. (Figure 1).
The most noticeable differences were observed between racial groups, with notably fewer HPV-positive SCCs in non-Hispanic Black persons (50.7%) compared with non-Hispanic White persons (73.6%), Hispanic persons (74.4%), or Asian Pacific Islanders (80.0%).
Other studies that noted similar differences by race/ethnicity found this to be a recent but ongoing development (28).
Settle et al. (29), who investigated oral cancer survival, also reported reduced HPV prevalence in Black persons compared with other race/ethnicity groups and found that this difference was particular to oropharyngeal cancer and not to other cancers of the oral cavity.
In addition to differences by race/ethnicity, HPV prevalence also varied by sex, particularly for HPV-16/18.
Prevalence was 66% among men, notably higher than the 53% found among women, which was a finding consistent with results of other investigations (2).
Although further data stratification might show even greater dissimilarities, for instance between Black women and White men, the sample sizes for these analyses were modest and confidence intervals were large (data not shown).
The precise causes for these discrepancies are unknown and most likely complex, but may be anticipated to influence vaccine efficacy for OPSCC.
Prevalence differences observed between the registry states may be, in part, caused by demographic variations.
Difference in age at diagnosis between patients with HPV-positive and HPV-negative cases was borderline significant (p = 0.023). Although other studies have also shown that HPV-positive cancers occur in a younger population (30), the role of 3 years difference in median age is unclear.
It is possible that differences in behavior associated with causal pathways, such as smoking and drinking, provide a partial explanation.
Persistent HPV infection at these anatomic sites may occur early, leading to more rapid and damaging alterations in cell cycle regulation and proliferation than those that occur with other carcinogenic exposures.
Of particular note, high-risk HPV types were detected in 80% of tonsillar SCCs.
The microanatomy of the lymphoepithelial tissue of Waldeyer’s ring, most notably the lingual and palatine tonsils, may explain this finding.
Deep invaginations in this area by the tonsillar crypts may expose immature basal cells to HPV (31).
The median age of case-patients was slightly lower than that of those with cancer in other sites (55 years), but proportions of infection, when sex and race/ethnicity were considered, were not different than proportions for the other oropharyngeal sites (data not shown).
One limitation of this study is that not all participating sites were able to perform systematic random sampling of case-patient specimens from their eligible pool.
The sizable specimen collections from the 4 cancer registries (Michigan, Kentucky, Louisiana, and Florida) were sampled by a simple random or systematic sampling approach, on the basis of the number of eligible cases.
Sampling from the SEER tissue repositories (Los Angeles, California; Hawaii; and Iowa) was dependent on what tissue specimens were available.
However, the resulting sample population that was ultimately tested represented diverse geographic regions and a wide range of demographic variables regarding sex, age, and race/ethnicity.
It should be noted that the presence of HPV DNA does not confirm its causal role in carcinogenesis.
Detection in tumor tissues potentially overestimates the true involvement of the virus because coincidental, transient infections and complementary transforming effects to other factors cannot be distinguished.
The natural history of cases in this study could not be assessed in this retrospective cross-sectional study and behavioral data were not available from the participating cancer registries.
In particular, information regarding tobacco or alcohol use and HIV status would potentially improve estimation of the proportion of OPSCC caused by HPV alone.
Because it is not clear at this point if HPV alone is sufficient to cause oropharyngeal cancer, factors other than use of tobacco products should be considered.
Additional HPV markers, such as viral transcription (particularly E6 and E7 mRNA) or characteristic gene expression profiling, may provide further insights in future assessments and show distinction between actively transforming HPV infections and random, transient occurrences (32,33). Similar investigations may also be warranted to explicate the 7 cases in which only low-risk types were found.
It is likely that these HPV types were present coincidentally and played no role in malignant transformation, but genomic changes that altered their pathogenic properties to bring them closer to those of high-risk types could provide an intriguing alternative explanation.
Conclusions
Future assessments are needed to monitor general prevalence and possible type-specific shifts.
Data from the present and future studies will provide a baseline for early assessment of vaccine effects.
Because the natural history and pre-cancer stages of oropharyngeal cancers are not established as they are for cervical cancer, direct trials with oropharyngeal neoplasia as the endpoint are not feasible.
To obtain meaningful, comparable data for this objective, researchers need a universal definition of the anatomic oropharynx and associated malignancies and agreement on laboratory methods.
Acknowledgments
We thank all members of the HPV Typing of Cancers Workgroup for their contributions toward this study.
Members of the HPV Typing of Cancers Workgroup are the following:
Battelle (Bruce Ellis, Arlington, VA, USA; Natalie Madero, Baltimore,
MD, USA; Emily Reid, Durham, NC, USA; Donna Little, Baltimore; April
Greek, Seattle, WA, USA; Dale Rhoda, Linda Delma Gieseke, Stephanie
Ashcraft, Columbus, OH, USA; Battelle Toxicology Northwest, Richland, WA
(Katherine Gideon); Carolinas Rehabilitation, Charlotte, NC (Tara
Ruhlen); Centers for Disease Control and Prevention, Atlanta, GA, USA
(Mariela Z Scarbrough, Trevor Thompson, Deblina Datta, Susan Hariri);
Louisiana State University, Baton Rouge, LA, USA (Lauren Cole); Michigan
Department of Community Health, Lansing, MI, USA (Lana Ashley, Jetty
Alverson, Michelle Hulbert, Won Silva); National Cancer Institute,
Rockville, MD (Sean Altekruse); St Joseph Mercy Hospital, Ann Arbor, MI
(Samuel Hirsch); University of Florida, Gainesville, FL, USA (Martha
Campbell-Thompson, Amy Wright, Kelley Durden); University of Miami,
Florida Cancer Data System, Miami, FL (Jill MacKinnon, Carlos Alvarez);
University of Hawaii, Cancer Research Center of Hawaii, Honolulu, HI,
USA (Hugh Luk, David Horio, Shoji Ikeda, Michael Green, Catherine
Grafel-Anderson, Rayna Weise); University of Iowa, Iowa City, IA, USA
(Freda Selk, Dan Olson); University of Kentucky, Lexington, KY, USA
(Thomas Tucker, Amy Christian); University of North Carolina Hospitals
Cancer Registry, Chapel Hill, NC (Susan Brossoie); and University of
Southern California, Los Angeles, CA, USA: Joe House, Myles G. Cockburn,
Andre Kim)
The collection of original specimens from nonrepositories (Kentucky,
Florida, Michigan, Louisiana), coordination of genotyping data from both
the Surveillance, Epidemiology, and End Results (SEER) program and the
National Program of Cancer Registries (NPCR) was largely supported by
CDC intramural funds and Vaccine For Children Funds.
This project has
been supported in part with federal funds by CDC under grant nos.
5U58DP000810-5 (Kentucky), 5U58DP000844-5 (Florida), 5U58DP000812-5
(Michigan), and 5U58DP000769-5 (Louisiana); and with federal funds for
Residual Tissue Repositories from the National Cancer Institute SEER
Population-based Registry Program, National Institutes of Health,
Department of Health and Human Services, under contract nos.
N01-PC-35139 (Los Angeles), N01-PC-35143 (Iowa), and N01-PC-35137
(Hawaii).
The collection of data from California used in this
publication was largely supported by the California Department of Health
Services as part of the statewide cancer reporting program mandated by
California Health and Safety Code Section 103885; by the National Cancer
Institute, National Institutes of Health, Department of Health and
Human Services, under contract no. N01-PC-2010-00035; and grant no.
1U58DP000807-3 from CDC. B.Y.H. has received consultation and speaker
fees from Merck and Co., Inc.
Dr Steinau is a microbiologist at the Centers for Disease Control and
Prevention (CDC) in Atlanta, Georgia, USA. He leads the human
papillomavirus DNA laboratory in the Chronic Viral Diseases Branch.
His
main interests focus on molecular methods for detection and
characterization of human papillomaviruses and associated diseases.
References
- de Martel C, Ferlay J, Franceschi S, Vignat J, Bray F, Forman D, Global burden of cancers attributable to infections in 2008: a review and synthetic analysis. Lancet Oncol. 2012;13:607–15 . DOI
 PubMed
PubMed
- Centers for Disease Control and Prevention (CDC). Human papillomavirus-associated cancers—United States, 2004–2008. MMWR Morb Mortal Wkly Rep. 2012;61:258–61 .PubMed

- Gillison ML. Human papillomavirus–associated head and neck cancer is a distinct epidemiologic clinical, and molecular entity. Semin Oncol. 2004;31:744–54. DOI
 PubMed
PubMed
- D'Souza G, Kreimer AR, Viscidi R, Pawlita M, Fakhry C, Koch WM, Case-control study of human papillomavirus and oropharyngeal cancer. N Engl J Med. 2007;356:1944–56. DOI
 PubMed
PubMed
- Martinez I, Wang J, Hopson KF, Ferris RL, Khan SA. Identification of differentially expressed genes in HPV-positive and HPV-negative oropharyngeal squamous cell carcinomas. Eur J Cancer. 2007;43:415–32. DOI
 PubMed
PubMed
- Miller DL, Puricelli MD, Stack MS. Virology and molecular pathogenesis of HPV (human papillomovirus)-associated oropharyngeal squamous cell carcinoma. Biochem J. 2012;443:339–53. DOI
 PubMed
PubMed
- Herrero R, Quint W, Hildesheim A, Gonzalez P, Struijk L, Katki HA, Reduced
prevalence of oral human papillomavirus (HPV) 4 years after HPV
vaccination in a randomized clinical trial in Costa Rica. PLoS ONE. 2013;8:e68329. DOI
 PubMed
PubMed
- Watson M, Saraiya M, Ahmed F, Cardinez CJ, Reichman ME, Weir HK, Using
population-based cancer registry data to assess the burden of human
papillomavirus-associated cancers in the United States: overview of
methods. Cancer. 2008;113(Suppl):2841–54. DOI
 PubMed
PubMed
- Gillison ML, Chaturvedi AK, Lowy DR. HPV prophylactic vaccines and the potential prevention of noncervical cancers in both men and women. Cancer. 2008;113:3036–46 . DOI
 PubMed
PubMed
- Fakhry C, Westra WH, Li S, Cmelak A, Ridge JA, Pinto H, Improved
survival of patients with human papillomavirus-positive head and neck
squamous cell carcinoma in a prospective clinical trial. J Natl Cancer Inst. 2008;100:261–9. DOI
 PubMed
PubMed
- Kreimer AR, Clifford GM, Boyle PB, Fransceschi S. Human papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic review. Cancer Epidemiol Biomarkers Prev. 2005;14:467–75. DOI
 PubMed
PubMed
- Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011;29:4294–301. DOI
 PubMed
PubMed
- Ryerson AB, Peters ES, Caughlin SS, Chen VW, Gillison ML, Reichman ME, Burden of potentially human papillomavirus-associated cancer of the oropharynx and oral cavity in the US, 1998–2003. Cancer. 2008;113:2901–9. DOI
 PubMed
PubMed
- Mirghani H, Moreau F, Lefèvre M, Tam C, Périé S, Soussan P, Human papillomavirus type 16 oropharyngeal cancer in lymph nodes as a marker of metastases. Arch Otolaryngol Head Neck Surg. 2011;137:910–4. DOI
 PubMed
PubMed
- Gargano JW, Wilkinson EJ, Unger ER, Steinau M, Watson M, Huang Y, Prevalence
of human papillomavirus types in invasive vulvar cancers and vulvar
intraepithelial neoplasia 3 in the United States before vaccine
introduction. J Low Genit Tract Dis. 2012;16:471–9. DOI
 PubMed
PubMed
- Steinau M, Unger ER, Hernandez BY, Goodman MT, Copeland G, Hopenhayn C, Human papillomavirus prevalence in invasive anal cancers in the United States prior to vaccine introduction. J Low Genit Tract Dis. 2013;17:397–403. DOI
 PubMed
PubMed
- Steinau M, Patel SS, Unger ER. Efficient DNA extraction for HPV genotyping in formalin-fixed, paraffin-embedded tissues. J Mol Diagn. 2011;13:377–81. DOI
 PubMed
PubMed
- Hariri S, Steinau M, Rinas A, Gargano J, Ludema C, Unger ER, HPV
genotyping in high grade cervical lesions and invasive cervical
carcinoma as detected by two commercial DNA assays, North Carolina,
2001–2006. PLoS ONE. 2012;7:e34044. DOI
 PubMed
PubMed
- Steinau M, Onyekwuluje JM, Scarbrough MZ, Unger ER, Dillner J, Zhou T. Performance of commercial reverse line blot assays for human papillomavirus genotyping. J Clin Microbiol. 2012;50:1539–44. DOI
 PubMed
PubMed
- Onyekwuluje JM, Steinau M, Swan DC, Unger ER. A real time PCR assay for HPV52 detection and viral load quantification. Clin Lab. 2012;58:61–6 .PubMed

- Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah K, Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189:12–9. DOI
 PubMed
PubMed
- Watson M, Lyu C, Unger ER, Copeland G, Peters E, Huang Y,
Centers for Disease Control and Prevention human papillomavirus typing
of cancers study with 7 registries: evaluating representativeness. North
American Association of Central Cancer Registries (NAACCR) Annual
Conference, 2011. Abstract, no. 58. http://www.naaccr.org/LinkClick.aspx?fileticket=udtv3Esreek%3d&tabid=257&mid=732

- Mehanna H, Beech T, Nicholson T, El-Hariry I, McConkey C, Paleri V, Prevalence
of human papillomavirus in oropharyngeal and nonoropharyngeal head and
neck cancer-systematic review and meta-analysis of trends by time and
region. Head Neck. 2013;35:747–55. DOI
 PubMed
PubMed
- Frisch M, Hjalgrim H, Jaeger AB, Biggar RJ. Changing patterns of tonisllar squamous cell carcinoma in the United States. Cancer Causes Control. 2000;11:489–95. DOI
 PubMed
PubMed
- Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009;45:309–16. DOI
 PubMed
PubMed
- Paolini F, Rizzo C, Sperduti I, Pichi B, Mafera B, Rahimi SS, Both mucosal and cutaneous papillomaviruses are in the oral cavity but only alpha genus seems to be associated with cancer. J Clin Virol. 2013;56:72–6. DOI
 PubMed
PubMed
- Gillison ML, Broutian T, Pickard RK, Prevalence of oral HPV infection in the United States, 2009–2010. JAMA. 2012;307:693–703. DOI
 PubMed
PubMed
- Brown LM, Check DP, Devesa SS. Oropharyngeal cancer incidence trends: diminishing disparities. Cancer Causes Control. 2011;22:753–63. DOI
 PubMed
PubMed
- Settle K, Posner MR, Schumaker LM, Tan M, Suntharalingam M, Goloubeva O, Racial
survival disparity in head and neck cancer results from low prevalence
of human papillomavirus infection in black oropharyngeal cancer
patients. Cancer Prev Res (Phila). 2009;2:776–81. DOI
 PubMed
PubMed
- Chaturvedi AK, Engels EA, Anderson WF, Gillison ML. Incidence trends for human papillomavirus-related and -unrelated oral squamous cell carcinomas in the United States. J Clin Oncol. 2008;26:612–9. DOI
 PubMed
PubMed
- Pai SI, Westra WH. Molecular pathology of head and neck cancer: implications for diagnosis, prognosis, and treatment. Annu Rev Pathol. 2009;4:49–70. DOI
 PubMed
PubMed
- Jung AC, Briolat J, Millon R, de Reyniès A, Rickman D, Thomas E, Biological
and clinical relevance of transcriptionally active human papillomavirus
(HPV) infection in oropharynx squamous cell carcinoma. Int J Cancer. 2010;126:1882–94.PubMed

- Sethi S, Ali-Fehmi R, Franceschi S, Struijk L, van Doorn L-J, Quint W, Characteristics and survival of head and neck cancer by HPV status: a cancer registry-based study. Int J Cancer. 2012;131:1179–86. DOI
 PubMed
PubMed
Figure
Tables
Suggested citation for this article:
Steinau M, Saraiya M, Goodman MT, Peters ES, Watson M, Cleveland JL, et
al. Human papillomavirus prevalence in oropharyngeal cancer cells before
vaccine introduction, United States. Emerg Infect Dis. 2014 Mon [date cited]. http://dx.doi.org/10.3201/eid2005.131311
1Members of HPV Typing of Cancers Workgroup who contributed to this study are listed at the end of this article.

Δεν υπάρχουν σχόλια:
Δημοσίευση σχολίου
Σημείωση: Μόνο ένα μέλος αυτού του ιστολογίου μπορεί να αναρτήσει σχόλιο.